Innovation in emergency medicine
CARL pushes back the boundaries of resuscitation therapy
Few people survive a cardiac arrest; blood stops flowing to the brain and other vital organs and the resulting lack of oxygen causes extensive damage to the body. In response to this, researchers at the University Medical Centre Freiburg and Resuscitec GmbH have developed CARL, an innovative resuscitation system, which – in addition to the oxygen level – adjusts numerous blood parameters to individual patient requirements. This greatly improves the chances of survival and reduces neurological damage.
In Germany, around 120,000 people suffer a sudden cardiac arrest (SCA) in a non-hospital setting every year.1) Only 11 percent survive, partly because resuscitation measures are often taken too late. However, even with the best care the heart does not always restart. 60 percent of people who have had a heart attack might experience sudden cardiac arrest due to significant heart damage. And even if the heart starts beating again, it is often so weakened that not enough blood and oxygen reach the brain. Toxic metabolites accumulate in the blood and cells during the standstill, which is why reperfusion usually causes further damage. The chances of survival in hospital are therefore quite low (20 percent) and a large proportion of survivors are left with severe neurological damage.
CARL - targeted extracorporeal reperfusion
 The innovative resuscitation system CARL (Controlled Automated Reperfusion of the whoLe body) was developed by Prof. Dr. Friedhelm Beyersdorf, Prof. Dr. Georg Trummer and Prof. Dr. Christoph Benk (from left to right) and their colleagues at the University Medical Centre Freiburg and Resuscitec GmbH. © University Medical Centre Freiburg
The innovative resuscitation system CARL (Controlled Automated Reperfusion of the whoLe body) was developed by Prof. Dr. Friedhelm Beyersdorf, Prof. Dr. Georg Trummer and Prof. Dr. Christoph Benk (from left to right) and their colleagues at the University Medical Centre Freiburg and Resuscitec GmbH. © University Medical Centre Freiburg"Thirty years ago, we were investigating whether it made sense to return unaltered blood to patients who had suffered sudden cardiac arrest. Such a line of enquiry did not take into account the pathophysiological causes," says Prof. Dr. Friedhelm Beyersdorf, former Medical Director of the Department of Cardiovascular Surgery at the University Medical Centre Freiburg. In decades of research, he and his colleague Prof. Dr. Georg Trummer, Head of Intensive Care Medicine, together with a large group of other researchers, first identified the therapeutic factors for successful reperfusion and then, together with Prof. Dr. Christoph Benk, Head of Cardiotechnology, developed a new type of small heart-lung machine specifically for resuscitation.
The therapy concept known as CARL - abbreviation for Controlled Automated Reperfusion of the whoLe Body - comprises seven different device units that work together to completely replace heart and lung function. Treatment is therefore independent of the underlying disease. Blood is taken from the large femoral vein and modified extracorporeally, i.e. outside the body, before being pumped back into the femoral artery. "Compared to conventional heart-lung machines, this allows us to correct the oxygen content of the stale blood as well as a total of 14 vital blood parameters," says Beyersdorf, describing the innovative technology. The doctors proceed very carefully, as damage caused by lack of oxygen is not easy to repair. Beyersdorf, a heart surgeon, explains: "For example, it is important not to supply too much oxygen at the start of reperfusion to prevent free radicals from forming and further damaging the mitochondria, which are the cells' energy power plants."
Comprehensive monitoring enables customised adjustment of blood parameters
CARL can also be used to adjust the concentration of carbon dioxide, various electrolytes such as calcium, potassium and sodium, blood acidity and a number of physical parameters. "We use a dual pump control system to generate a pulsatile blood flow," explains engineer Benk. "One pump guides the blood through the artificial lung, while the other accelerates it to make the blood flow pulsate as it would under physiological conditions." This significantly increases the blood pressure, ensuring the brain is adequately supplied with blood despite the fact that the cells of the inner vessel wall swell considerably after a cardiac arrest has occurred. "With the help of a newly designed cooling unit, we can also lower the temperature of the returning blood so that the patient's body quickly cools to around 33 °C . This helps to slow down the metabolic processes."
A key aspect of the procedure is the ability to conduct extensive real-time measurements of all parameters during treatment, enabling the therapy to be quickly adapted to a patient’s individual circumstances. This is crucial because each patient’s initial situation is unique and each patient reacts differently to the measures taken.
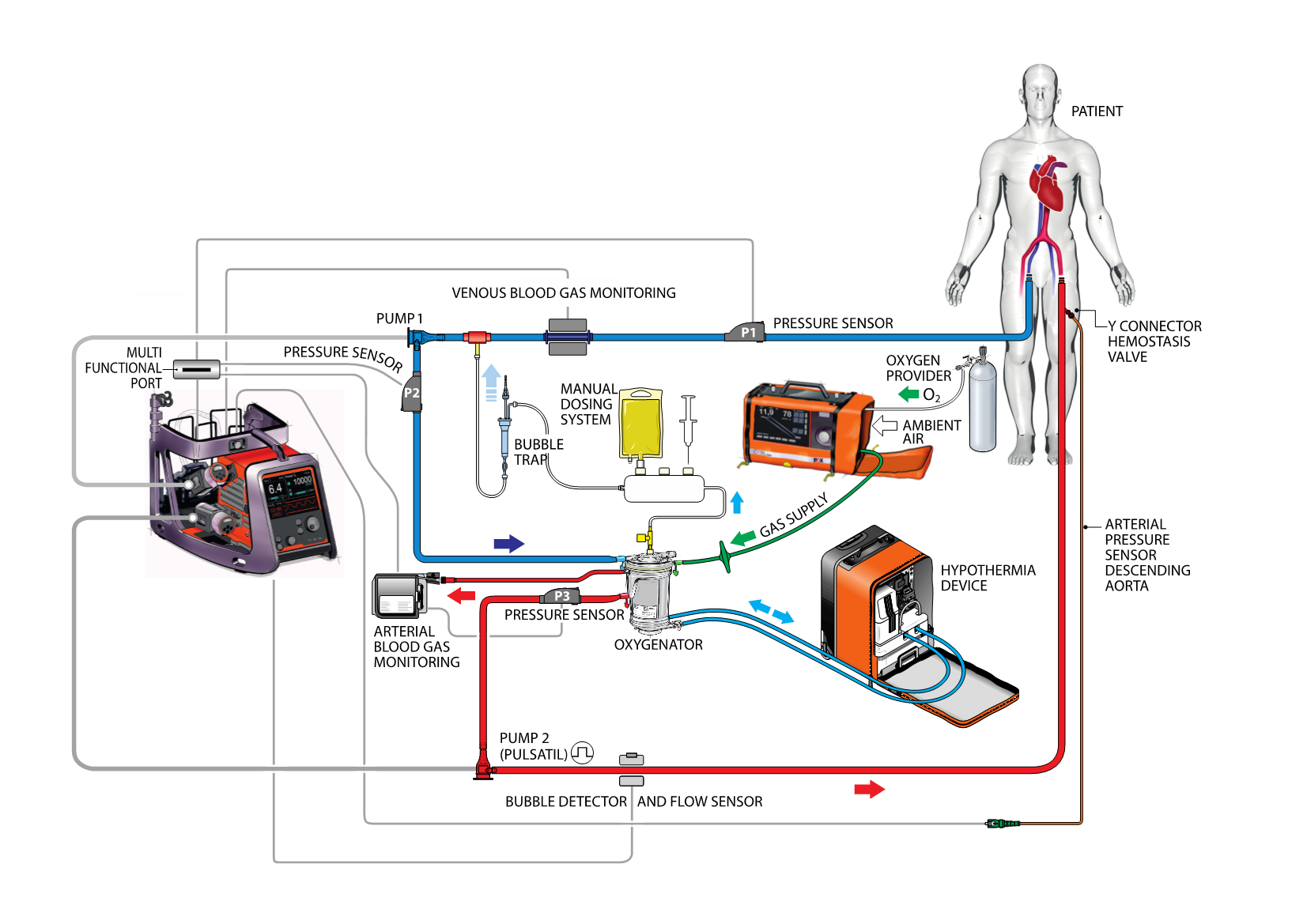 Schematic representation of the CARL therapy concept. The blood taken from the femoral vein goes through numerous analyses in an extracorporeal circuit (e.g. blood gases, blood pressure, electrolyte content), cooled and returned via the femoral artery with adjusted parameters. Source: https://doi.org/10.3390/jcm13010056, Georg Trummer, CC-BY 4.0 (https://creativecommons.org/licenses/by/4.0/)
Schematic representation of the CARL therapy concept. The blood taken from the femoral vein goes through numerous analyses in an extracorporeal circuit (e.g. blood gases, blood pressure, electrolyte content), cooled and returned via the femoral artery with adjusted parameters. Source: https://doi.org/10.3390/jcm13010056, Georg Trummer, CC-BY 4.0 (https://creativecommons.org/licenses/by/4.0/)
Spin-off Resuscitec GmbH
When they first began the project, the researchers used existing technologies and tested the method in animal models. Benk explains: "Back then, the system we used was almost too big to fit in a room. Nevertheless, we successfully carried out the first therapies." Resuscitec GmbH was then founded in 2010 to transfer the basic research results into a small and, above all, mobile technology. Trummer explains: "Time is a crucial factor, especially as far as sudden cardiac arrest is concerned. The portable therapy system can easily be brought to the bedside. And even more importantly, if an SCA patient arrives at a hospital by ambulance – which is usually the case – the portable system makes it possible to start treatment immediately.”
The company, which currently has 60 employees, has developed a total of seven different medical devices, all of which have been approved for clinical use since 2020. By merging various devices into one unit and using carbon fibre, both the size and weight (now only 18 kg) was significantly reduced. CARL now easily fits into a vehicle and can also be attached to a stretcher.
Two to three times higher chance of survival with good neurological function
 The CARL technology includes the CARL controller, CARL MOX for O2 and CO2 control and the CARL COOLER cooling unit. © Resuscitec GmbH
The CARL technology includes the CARL controller, CARL MOX for O2 and CO2 control and the CARL COOLER cooling unit. © Resuscitec GmbHA European-wide study2) published in December 2023 in the renowned Journal of Clinical Medicine clearly demonstrates the impressive success of the innovative therapy concept. First author Trummer explains: "We tried to reflect reality, which is why this was an observational study with no strict inclusion and exclusion criteria." Accordingly, the device was also used on the over-80s and people with a very poor initial situation.
A total of 69 patients aged between 21 and 86 were treated in seven specialised centres in Germany, Austria and the Netherlands between January 2020 and January 2023. The overall survival rate was 42 percent (or 48 percent if the nine non-survivable cases with aortic rupture or torn myocardium were excluded). Almost 52 percent of those affected survived if they had a cardiac arrest while hospitalised. Outside a hospital setting, 35 percent of those who had a cardiac arrest survived. However, if they were connected to CARL before they were admitted to hospital, their chance of survivalincreased to 57 percent.
Remarkably, the majority of survivors (80 percent) had little or no neurological impairment (CPC 1-2, Cerebral Performance Category). And even in a third of those discharged from hospital as CPC-3 cases, their condition improved significantly within 90 days.
"All the patients that experienced SCA would not normally have survived," says Trummer. Beyersdorf adds: "Our therapy is only used if the heart cannot be restarted with conventional resuscitation measures. CARL is at the end of the rescue chain." Previously, the chance of survival after 20 to 30 minutes of resuscitation was almost zero. With the help of the new procedure, all patients survived beyond this time, and some were even saved after more than 60 minutes of resuscitation.
Award-winning therapy concept
The ambitious project required a great deal of stamina from the researchers involved. However, CARL is now in use throughout Europe and is also due to be approved for the US market.
In 2023, Resuscitec and the University Medical Centre Freiburg won the Lothar Späth Award for Innovative Developments from Baden-Württemberg and Thuringia. They were honoured with the award because CARL specifically addresses an individual’s condition after acute cardiac arrest and thus pushes back the boundaries of resuscitation.