Open wounds are usually covered with suitable wound dressings to protect them against infection and absorb secretions. Traditional dry wound dressings such as plasters or gauze usually suffice to cover minor injuries or surgical sutures. However, chronic, non-healing wounds or larger, gaping injuries require more comprehensive treatment involving, for example, interactive dressings that contain hydrocolloids, alginates or hydrogels, or that consist of polyurethane foam. These materials create a moist and warm environment that enhances the migration of immune and tissue cells, thus promoting the healing process.
EU-wide WOUNDSENS project
 Kai Fuchsberger (left) and Dr .Ruben Daum (right) are developing novel sensory nanofibres in the NMI’s Regenerative Biomaterials working group led by Dr. Hanna Hartmann (centre). © Janine Hartmann Photography; Michael Fuchs Photography
Kai Fuchsberger (left) and Dr .Ruben Daum (right) are developing novel sensory nanofibres in the NMI’s Regenerative Biomaterials working group led by Dr. Hanna Hartmann (centre). © Janine Hartmann Photography; Michael Fuchs Photography"Current methods for assessing the infection status of wounds involve visual inspection, which requires bandages to be removed completely," explains Kai Fuchsberger from the NMI Natural and Medical Sciences Institute at the University of Tübingen in Reutlingen. "This can be very painful and may also damage newly formed tissue. Wound dressings that provide information on the condition of the wound to the outside world would therefore be highly beneficial." This could potentially be done by electrochemical sensors. However, there is one drawback: they are small, sharp-edged plastic components with electrodes attached. "No one wants that kind of thing in a wound," says Fuchsberger, a biologist who specialises in electrochemistry. "We therefore discussed the possibility of producing something like a fleece that could function as a sensor. We envisaged something that looked like a traditional wound dressing."
The first thing required to make a product of this kind is a biomarker, i.e. a substance that occurs in the wound that could be used as an indicator for inflammation-dependent changes. The substance would be quantified using specific enzymes – based on the generation of a current flow. Amperometric biosensors of this kind are currently used in laboratories to determine cholesterol or glucose, among other things. However, before such amperometric biosensors can be used for monitoring the wound status, the enzymes would need to be included in a flexible dressing material and remain stable under everyday conditions for a prolonged period of time. The NMI, along with the two other WOUNDSENS partners, is planning to produce an initial prototype. The WOUNDSENS project has been running since November 2023 and is funded by the EU Horizon 2020 programme (FKZ 101115337). EvoEnzyme, a Madrid-based company, is in charge of adapting the enzyme to the product requirements while the University of Lorraine’s Institut Jean Lamour is developing the conductive material.
Versatile nonwoven production using electrospinning
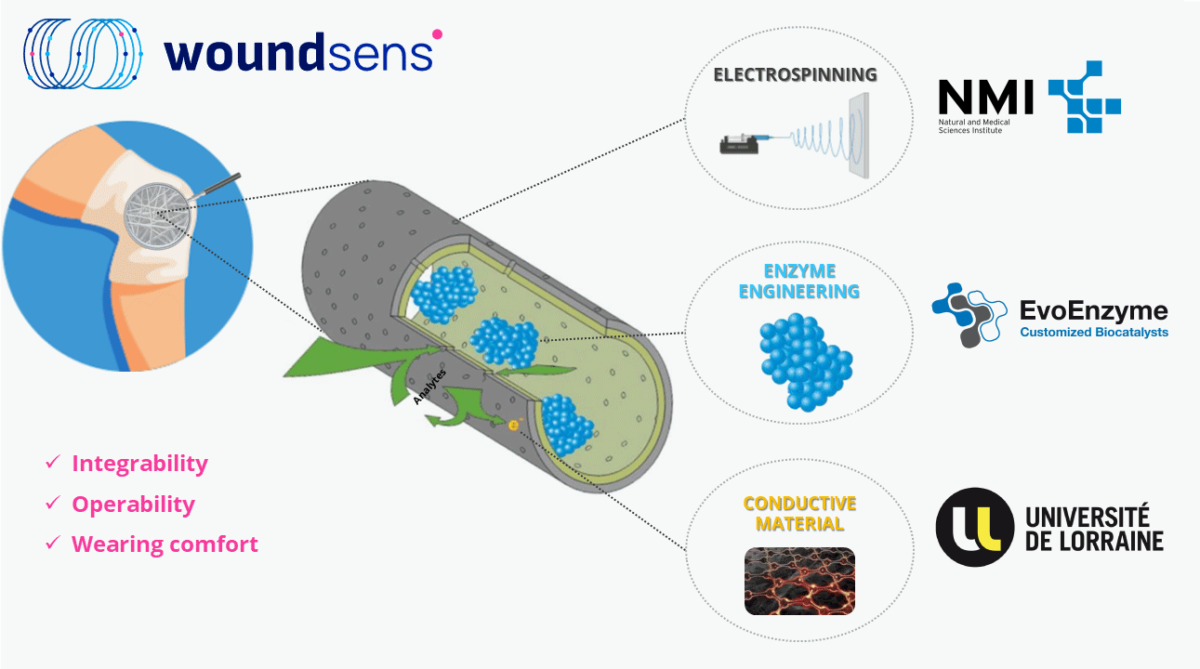 As part of the European WOUNDSENS project, hollow fibres containing enzymes will be spun into sensory wound dressings. © 2023 WOUNDSENS
As part of the European WOUNDSENS project, hollow fibres containing enzymes will be spun into sensory wound dressings. © 2023 WOUNDSENSThe Regenerative Biomaterials working group at the NMI, headed up by Dr. Hanna Hartmann, is in charge of developing suitable fibres to be used as the basis for sensory wound dressings. The researchers will be using a process known as electrospinning, which was established at the NMI many years ago. "This method produces very fine fibres ranging from a few hundred nanometres to a few micrometres in diameter," explains Dr. Ruben Daum, who gained in-depth experience in this field during his doctorate. In many cases, a dissolved plastic polymer is used as the starting material, which is then pumped through a metal needle using a syringe. The application of voltage (5-30 kV) between the metal needle and a collector on the other side, electrostatically charges the emerging polymer, which is thus drawn towards the earthed collector. The solvent evaporates during the process, causing the plastic to be deposited on the surface of the collector in the form of a wafer-thin, fleece-like thread.
"It is a relatively simple method that offers many possibilities depending on the material used and the shape of the collector," Daum explains. "The fleece can be spun into any shape." And as it is similar in structure to the extracellular matrix of body tissue, it is ideally suited as a biomaterial for medical products.
Sensory wound dressings made from special hollow fibres
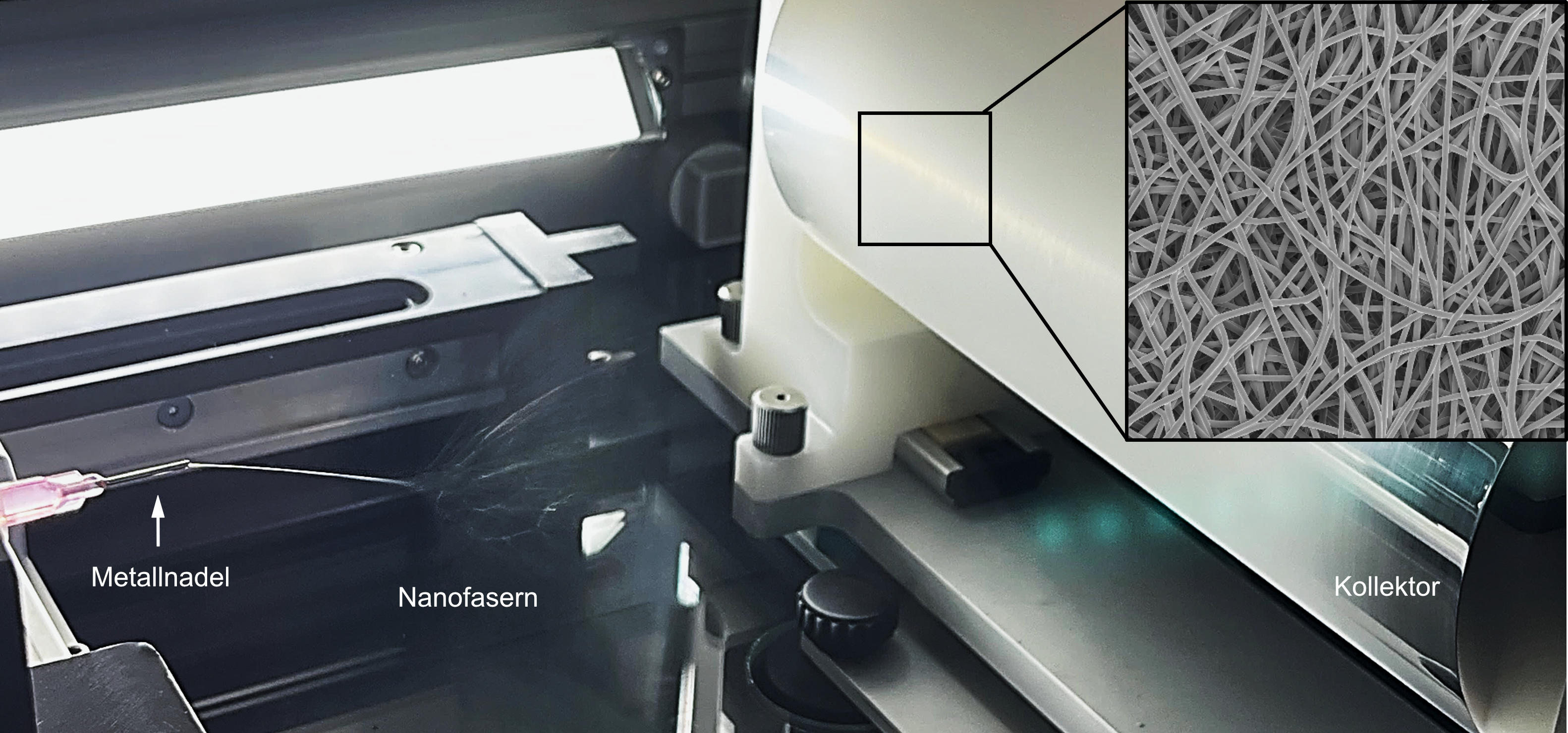 In electrospinning, the fiber material is drawn from the tip of a metal needle (left) onto a rotating collector (right) when a high voltage is applied, where it is deposited as a wafer-thin, continuous thread (magnification top right). © NMI Reutlingen
In electrospinning, the fiber material is drawn from the tip of a metal needle (left) onto a rotating collector (right) when a high voltage is applied, where it is deposited as a wafer-thin, continuous thread (magnification top right). © NMI ReutlingenElectrospinning is not something fundamentally new when it comes to producing wound dressings. Daum explains in greater detail: "But what we want to do here is generate hollow fibres that contain enzymes." The researchers will use so-called coaxial needles in which a very thin needle is placed inside a slightly larger needle. The polymer solution is transported in the space between the inner and outer needle, while the carrier material with the dissolved enzyme is inside the inner needle, allowing both parts to be spun coaxially together. "The result is hard to predict due to the complex interaction of many factors including humidity, temperature, tension and flow rate. We will therefore have to fine-tune these parameters and optimise the process empirically," says Daum, explaining the challenges involved.
Care needs to be taken not to damage the enzyme during the sensory coating production process. Fuchsberger is optimistic: "Even though large electric fields are involved and the enzyme comes into direct contact with the liquid polymer solution, the process is very quick. Compared to conventional biosensors with immobilised enzymes, our method uses mobile enzymes inside the hollow fibres. We are hoping that this innovative method will increase enzyme activity." High sensitivity can also be expected due to the good surface-to-volume ratio and the associated large reaction area.
Relief for the healthcare system
It was important for the NMI group to first conduct interviews with patients and medical staff, as every wound is different and there are many different treatment options. Sensory fibres are not suitable for dry wounds, for example, as moisture is required for electricity to flow.
However, the innovative wound dressing could significantly improve treatment for chronic, weeping wounds, burns or surgical wounds that are difficult to access. Dressings are currently changed at least every 2-3 days; it will probably be possible to leave the sensory material on a wound for as long as 5-7 days. This would favour the healing process and greatly benefit both those affected and the healthcare system.
Data will be recorded via a chip attached near the wound and passed on to medical staff via Bluetooth. Staff will be able to react promptly in the event of pathological changes. In the long term, a telemedical application is also conceivable.